This article serves as the introduction to a series on Para-phenylenediamine (PPD): its health risks, history, and politics. In the coming weeks, articles will be published which explore each section in greater detail.
Para-phenylenediamine, or a chemically related -diamine is an ingredient used in virtually all oxidative hair dyes, both store-bought and used in salons. The oxidative dye process is formulated to quickly penetrate and stain the hair strand any color, including lightening hair by removing the pigment from the core of the hair and dyeing over it. Brunette and black hair dyes contain higher concentrations of PPD, though all colors can contain PPD.
Para-phenylenediamine can present a multitude of health risks if it is inhaled or if it comes in contact with skin. Despite a well-documented history of allergic reaction, sensitization, increased risk of cancer, and other serious health risks, it continues to be allowed in hair dyes at a maximum of 6% concentration in the United States.
The rate of PPD sensitization is increasing, but many doctors, hairstylists, and consumers remain unaware or apathetic. A lack of knowledge about PPD leads to continuation of serious reactions for people who use products containing PPD and related ingredients. It also allows companies which manufacture and sell products containing PPD to do so with relatively no regulation nor legal repercussion.
Educating consumers about the dangers of PPD and safer alternatives is becoming an increasingly important mission at Ancient Sunrise®.
1. PPD is highly sensitizing, and studies link it to lupus, non-Hopkins lymphoma and asthma. Allergic reactions can cause severe injuries, and can be fatal.
The hazards of para-phenylenediamine have been known since its introduction for use as an industrial fur dye, and in personal hair dyes. Academic articles from as early as 1915 warn against it. Symptoms of allergic reactions to para-phenylenediamine may include itching, swelling, hives, blistering, depigmentation, and permanent scarring; the reaction is a delayed hypersensitivity reaction, often occurring 3 to 30 days after application, so they are frequently misdiagnosed.
There have been an increasing number of fatal anaphylaxis reactions to PPD hair dye in recent years, particularly when people have previously had a PPD ‘black henna’ temporary tattoo. The allergic reactions often require emergency treatment to keep airways open, and further treatment in an ICU or burn ward. A person may additionally experience difficulty breathing and swelling of body parts near the site of exposure. In the case of hair dye use, this means swelling of the face, eyes, and throat. Reactions near the eyes can cause damage and loss of sight.

In countries where products with high PPD levels are easily accessible, ingesting hair dye is a known method of suicide and murder; women can generally purchase hair dye without arousing suspicion. Ingestion of PPD can lead to respiratory distress, rhabdomyolysis (muscle death), and renal failure.
PPD exposure has been linked to increased chances of certain cancers as well as asthma and non-Hodgkins lymphoma. Despite all this, PPD is legal for use on hair within the United States at up to a 6% concentration. Cosmetics companies continue to tout PPD as a safe ingredient despite decades of research, case studies, and hospitalizations.
2. There is no requirement to disclose the concentration percentage of PPD in products manufactured in the US.
Regulation of PPD varies greatly by country. The United States limits PPD to up to a 6% concentration in hair dye. The FDA differentiates between products used for hair coloring, and products applied directly on the skin because hair dyes are supposed to be used off the scalp and washed away after a period of time. In reality, those who apply hair dye at home will apply the product to the scalp, and will not always follow processing time instructions.
Even when these products are applied correctly, there is no guarantee that the customer will not develop a sensitization or a reaction. The dye may drip onto the scalp, face, neck or ears during processing time. For some, this brief contact with a low concentration may be all that it takes.
Other countries have a higher limit or no limit at all on concentration levels. These products are easy enough to purchase over the internet. They can also be found at international grocery stores. When hair dye is sold in powder form, concentration is directly dependent on the amount of water mixed with the powder. One study found that packages of black hair dye manufactured in India and China (often sold as black henna) contained 12.5% to over 30% PPD, far in excess of legally allowed levels. Other samples have been found to have as high as 60% PPD.
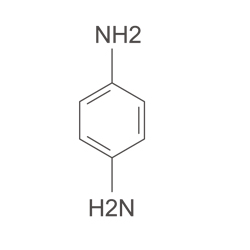
3. “Black Henna” body art is not henna. It is illegal, but laws are not well enforced.
“Black henna” appeared in the United States and flourished seemingly overnight in the 90’s, spurred by Madonna’s “Frozen” music video released in 1998. in the video, her hands are decorated with black henna patterns. These were done with Bigen black hair dye at the Ziba salon in Los Angeles. Based on first injury reports, it can be estimated that henna artists from South Asia have been using high PPD black hair dye since the 1980’s as “black henna.” Pop-up stalls in tourist locations offered temporary body art that stained the skin black very quickly, and lasted for two to four weeks. “Black henna” created the illusion of a real tattoo without the permanence or pain (unless one experiences a reaction). Black henna body artists were transient and often unaware of the dangers of their own materials.

Within the United States and most countries, PPD is illegal for direct use on skin unless it is for cultural purposes. While imported shipments of “black henna” body art products are regularly seized by customs, it is easy enough to purchase hair dyes containing PPD, which are not subject to seizure, and to use them on the skin. Dyes from countries with more lenient laws may report only “color powder” as an ingredient. Some international brands of popularly used for “black henna” body art contain as high as 30% PPD concentration, more than enough to sensitize an unsuspecting client in one exposure. A solid form of pure PPD is sold as “henna stone” from the banks of the Nile River, which creates instant black results for body art. This leads uninformed buyers to believe that a) the product is natural and safe; and b) that natural henna produces a black stain.

The use of high concentrations of PPD for henna-like body art gained popularity first in East Africa in the 1970’s. The product was less expensive and required an easier preparation than natural henna. It provided instant, black results which mimic the look of a permanent tattoo, and are more visible on darker skin tones. This practice then moved into Western countries, especially in high tourism areas.

Enforcing laws against the use of PPD on skin would require law enforcement officials to patrol high tourism areas such as beach fronts and piers where stalls are often set up. These stalls are transient, closing and opening in new locations. A solo artist could set up and work out of a toolbox, moving throughout the day. As mentioned earlier, many products containing high concentrations of PPD are not properly labeled, making it even more difficult to enforce bans.
In many cases, by the time a customer experiences a reaction to their “black henna” body art, the artist has long moved on to a new location, making it near impossible for health professionals to acquire a sample of what was used on the customer’s skin.
Www.mehandi.com sells Temptu professional-grade skin paint, which does not stain the skin and does not contain PPD, but which is water-resistant and can mimic the look of a black tattoo for up to seven days.
For more information about “black henna” tattoos and their dangers, visit http://www.hennapage.com/henna/ppd/index.html.
4. PPD sensitization can happen to anyone.
Research has shown that with enough exposures to high enough concentrations of PPD, anyone will develop a sensitization to PPD. In a well known study, 100% of subjects exposed to 10% concentrations of PPD developed a reaction within five patch tests. Rate of sensitization varies greatly among individuals. For some, it may take only one exposure to a lower concentration. Though the oxidative hair dye industry claims that fewer than 3% of people are allergic to hair dye, many studies have shown that number to be higher, and coroner Geoff Fell estimates that 14% of people are allergic to oxidative hair dye.
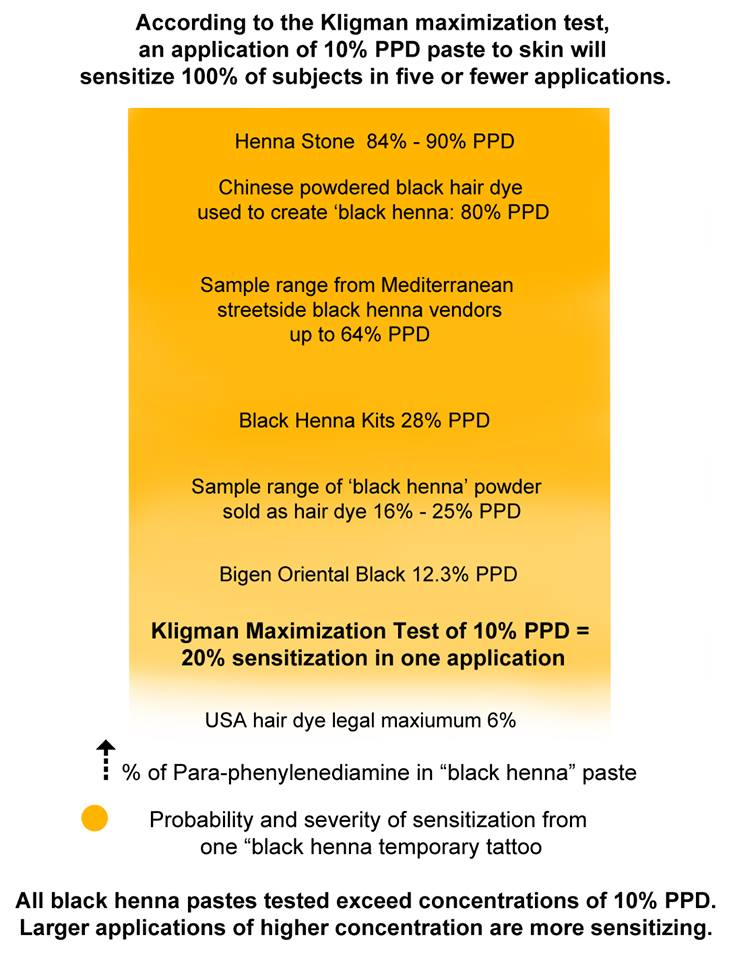
“Black henna” artists use a mixture that is 15% PPD or more. The chances of becoming sensitized to PPD after getting a “black henna” tattoo is about 50% Once sensitized, a person will experience a reaction the next time they come in contact with PPD. Of the people who are sensitized to PPD from a “black henna” tattoo, about 40% will experience a severe reaction upon their next exposure. This might be another “black henna” tattoo, or it could be years later, when that person decides to dye their hair. Even if the first exposure did not cause any reaction, the body can still have become sensitized. The next time this person comes in contact with PPD, they may experience a severe reaction without any understanding of the cause.
People who work in professions that require frequent contact with PPD can quickly develop sensitivities. Hair stylists who become PPD sensitive can no longer work at a traditional salon without experiencing reactions. PPD was once also used in fur-dyeing, leading to high rates of sensitization in fur industry workers.
5. Those who develop sensitivities to PPD may experience worsening symptoms with each exposure.
Reactions are not always immediate and severe. Oftentimes, reaction symptoms start out mild and worsen each time a person makes contact with the compound. A person who has dyed their hair using an oxidative dye for several years may at first experience no reaction, then one day notice some itching or burning, or have puffy eyes after applying hair dye. The next application might cause more painful symptoms. Before long, that person could require emergency hospital care for a reaction that has caused intense swelling to the entire face and head, and difficulty breathing.
Actor Pauley Perette had a typical progression of reaction: she had dyed her blonde hair black for twenty years, and the allergic reactions presented progressively until it was life-threatening. Follow the link here for additional news articles about PPD reactions.
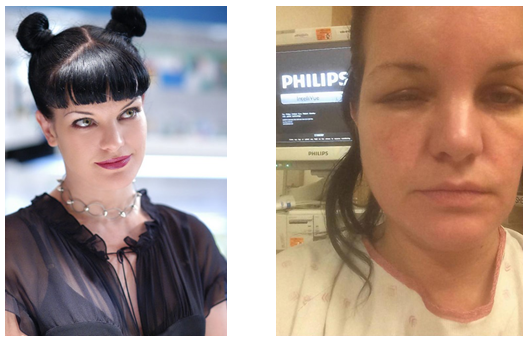
In 2012, a woman in the UK died after experiencing a reaction to an over-the-counter hair dye. Further investigation discovered she had previously gotten a “black henna” tattoo, which likely had sensitized her to future encounters with PPD. While this is an extreme case, it is not at all uncommon for people to become sensitized via exposure to a high concentration of PPD from a “black henna” tattoo, and go on to later use a dye containing PPD. People can become sensitized without experiencing an initial reaction. Those who do experience a reaction from “black henna” tattoos are usually unaware that commercial hair dyes contain the same ingredient.
One study discovered that even after participants were determined by way of patch test to have a PPD sensitivity, more than half continued to use hair dyes anyway. These participants were ones who experienced more mild reactions; those with severe reactions reported stopping hair dye. This shows that the average patient does not take their sensitization seriously, and is willing to endure a mild reaction for the sake of maintaining their desired hair color.
6. PPD sensitization can lead to cross-sensitization to related compounds.
Para-phenylinediamine is an aromatic amine in the benzodiamine family. Studies have shown that those with PPD sensitizations may also be sensitive to other benzodiamines, toluenediamines, analgesics such as benzocaine and lidocaine, azo-dyes, and PABA (para-aminobenzoic acid). The FDA lists examples of cross-sensitization here.
Hair dyes that are labeled “PPD free” may contain para-toluenediamine, a compound similar enough to elicit reactions for those who have PPD sensitivities, causing “PPD free” hair dyes to be just as problematic.
Unless tested in a clinical setting, it is unlikely that the average person who is sensitized to PPD will be aware of cross-sensitizations. This leaves them vulnerable to reactions from other sources, such as fabric dyes, cosmetics, black rubber (like that used to create car tires) pain relieving and numbing agents both administered in a hospital and bought over-the-counter, and even sunblock lotion.
Those who experience reactions from cross-sensitization may be frustrated and confused as to what is causing their allergies, and what products to avoid. A doctor may recognize a PPD sensitization and recommend their patient to stop using hair dyes containing PPD; however, if a patient has an unknown cross-sensitization, they may continue to present with similar symptoms without realizing the link.
7. The rate of PPD sensitization is growing.
The combination of an increased use in hair dye among younger people, and the explosion of the “black henna” industry in tourists areas has allowed for a jump in the rate of PPD sensitization. The most common source of sensitization for children and young adults is “black henna” tattoos. As mentioned above, the concentration of PPD in products used for “black henna” is extremely high, leading to a higher likelihood of sensitization in comparison to exposure to lower concentrations. This creates a population of youth who have already become sensitized prior to their first use of oxidative hair dye.
Studies have shown that people are using hair dye at younger ages and at higher frequencies. While hair dye was once more commonly used to mask gray hairs that came with age, it is now a common cosmetic tool to change hair color on a whim, regardless of age.
It is projected that by 2030, about 16% of middle class people in the UK, US, Australia, Korea, Japan, and Europe will be sensitized to PPD. The majority of this sensitization will have been caused by “black henna” tattoos gotten while on vacation. Rates will be higher in the Arabian Peninsula, East Africa, Muslim populations in Africa, and South Asia, where black henna has been used in weddings and for Eid. As the younger, “black henna” sensitized population reaches the age for graying hair, there will be a dramatic increase of PPD-related injury from hair dyes.

8. International “henna” for hair, and “natural” hair dye products are loosely regulated, and can contain PPD regardless of labeling.
Standards for ingredient disclosure vary depending on the country of origin. In countries like India, manufacturers are not required to disclose their full list of ingredients on products such as hair dye. Henna for hair products can be labeled as “pure” and “all natural” but in reality include PPD, metallic salts, and other chemical adulterants. Some products labeled “henna” can include little to no henna at all. “Henna” becomes a vague, catch-all term for supposedly natural hair products, regardless of the existence of lawsonia inermis plant powder contained therein. These compound hennas are then mistaken for safe BAQ henna.
It is an incorrect assumption that a product originating from South Asia, the Middle East, or other regions in which henna grows is automatically safe and natural. It is often the case that these products are the most adulterated.

9. Cosmetics companies that use PPD have little legal responsibility for PPD-related injuries.
US-based and international cosmetic giants which manufacture oxidative hair dyes containing PPD are relatively safe from litigation. They are required by the FDA to advise customers to conduct a patch test before using their products, and to avoid use if one has an allergy to “black henna.” This warning, along with the sheer size and strength of these companies, prevents successful legal action against them in the case of PPD-related injury. The lobbying power of these companies prevent the government from passing more stringent legislation on PPD. Current law does not require that injuries caused by hair dye reported to the manufacturer be made public, as this is regarded as financially sensitive information.
Dupont, the patent holder, explicitly absolves itself from harm done by any use that involves contact with skin.
“DuPont does not recommend and will not knowingly offer or sell p-phenylenediamine (PPD) for uses involving prolonged skin contact. Such uses may involve, but are not limited to, products formulated with henna for tattoo applications or other skin coloration effects. This use of PPD in prolonged skin contact application has the potential to induce allergic skin reactions in sensitive individuals.
Persons proposing to use PPD in any formulation involving any more than incidental skin contact must rely on their own medical and legal judgment without any representation on our part. They must accept full responsibility for the safety and effectiveness of their formulations.”
10. 100% pure henna is a safe, effective, and permanent alternative to oxidative hair dyes.
More and more people are seeking safer, natural cosmetic alternatives regardless of whether or not they have a sensitivity to ingredients in commercial products. Consumers are concerned about the environment and their own bodies. Using henna and related plant dye powders to dye hair is a process that requires more patience and knowledge than picking up a box of oxidative dye at the local store, but will yield permanent results without damage to the hair or body. It is essential that consumers insist on only henna products of the highest quality and purity. This means products that have been tested for PPD, metallic salts, and other harmful adulterants.

They can be used on all types of hair, and produce virtually any natural shade.
The practice of using plant powders to color the hair is centuries old. The knowledge of their use was once as commonplace as knowing how to drive a car is now. This can become the case again. It requires the availability of quality product, accurate information, and the dissemination of that information within and across communities through direct relationships and social networking. A common reason for being hesitant about using henna is that it seems complicated and time-consuming, but a great number of henna-users report that it becomes second nature, that they enjoy the process, and that the results are superior to boxed dyes.

Ancient Sunrise® provides quality products, information based in research, and a team of customer service representatives that are available through several avenues of communication. We have thousands of customers all over the world. We look forward to helping you on your journey to beautiful hair and healthier practices.
References
Almeida, Pablo J., Leopoldo Borrego, and José M. Limiñana. “Age‐related sensitization to p‐phenylenediamine.” Contact dermatitis 4, no. 3 (2011): 172-174.
Al-Suwaidi, Ayesha, and Hafiz Ahmed. “Determination of para-phenylenediamine (PPD) in henna in the United Arab Emirates.” International Journal of Environmental Research and Public Health 7, no. 4 (2010): 1681-1693.
Brancaccio, Ronald R., Lance H. Brown, Young Tae Chang, Joshua P. Fogelman, Erick A. Mafong, and David E. Cohen. “Identification and quantification of para-phenylenediamine in a temporary black henna tattoo.” American Journal of Contact Dermatitis 13, no. 1 (2002): 15-18.
Cartwright-Jones, Catherine. “The effect of black temporary tattoos on the chemical cosmetic industry and a solution to the problem.”Sofw Journal 143 (2017): 24-30.
Chen, Weiyang, Thobile AN Nkosi, Sandra Combrinck, Alvaro M. Viljoen, and Catherine Cartwright-Jones. “Rapid analysis of the skin irritant p-phenylenediamine (PPD) in henna products using atmospheric solids analysis probe mass spectrometry.” Journal of pharmaceutical and biomedical analysis 128 (2016): 119-125.
Fisher, Alexander A., Alfred Pelzig, and Norman B. Kanof. “The Persistence of Allergic Eczematous Sensitivity and the Cross-Sensitivity Pattern to Paraphenylenediamine** From The Department of Dermatology and Syphilology of the New York University Post Graduate Medical School (Dr. Marion B. Sulzberger, chairman) and The Skin and Cancer Unit of the New York University Hospital.” Journal of Investigative Dermatology 30, no. 1 (1958): 9-12.
Hashim, M. Sir, Y. O. Hamza, B. Yahia, F. M. Khogali, and G. I. Sulieman. “Poisoning from henna dye and para-phenylenediamine mixtures in children in Khartoum.” Annals of tropical paediatrics 12, no. 1 (1992): 3-6.
Hueber-Becker, Frédérique, Gerhard J. Nohynek, Eric K. Dufour, Wim JA Meuling, Albertus Th HJ de Bie, Herve Toutain, and Hermann M. Bolt. “Occupational exposure of hairdressers to [14 C]-para-phenylenediamine-containing oxidative hair dyes: A mass balance study.” Food and chemical toxicology 45, no. 1 (2007): 160-169.
Jacob, Sharon E., and Bruce A. Brod. “Paraphenylenediamine in black henna tattoos: sensitization of toddlers indicates a clear need for legislative action.” The Journal of clinical and aesthetic dermatology 4, no. 12 (2011): 46.
Jenkins, David, and Elizabeth T. Chow. “Allergic contact dermatitis to para‐phenylenediamine.” Australasian Journal of Dermatology 56, no. 1 (2015): 40-43.
Kligman, A. M. 1966. “The identification of contact allergens by human assay. 3. The maximization test: a procedure for screening and rating contact sensitizers.” Journal of Investigative Dermatology, v. 47 issue 5, p. 393-409. (1966)
McFadden, John P., Ian R. White, Peter J. Frosch, Heidi Sosted, Jenne D. Johansen, and Torkil Menne. “Allergy to hair dye.” BMJ: British Medical Journal 334, no. 7587 (2007): 220.
Özkaya, Esen, Kurtulus D. Yazganoglu, Aysem Arda, Zeynep Topkarci, and Erol Erçag. “The “henna stone” myth.” (2013).
Paley, Kristina, Larisa J. Geskin, and Matthew J. Zirwas. “Cutaneous B-cell pseudolymphoma due to paraphenylenediamine.” The American journal of dermatopathology 28, no. 5 (2006): 438-441.
Seidenari, Stefania, Lucia Mantovani, Bianca Maria Manzini, and Marco Pignatti. “Cross‐sensitizations between azo dyes and para‐amino compound.” Contact dermatitis 36, no. 2 (1997): 91-96.
Wilbert, M. I. “Cosmetics as Drugs.” Pub. Health Rep. 30, no. Oct. 15 (1915): 3059.
Rapid analysis of the skin irritant p-phenylenediamine (PPD) in henna products using atmospheric solids analysis probe mass spectrometry, Weiyang Chena, Thobile. A.N. Nkosia, Sandra Combrincka, Alvaro. M. Viljoena, Catherine Cartwright-Jones. Journal of Pharmaceutical and Biomedical Analysis, Volume 128, 5 September 2016, Pages 119–125


Great article. Will be sharing.
Thanks! 🙂
Thank you for writing this article. I appreciate the subject too.